Today’s blog post comes from Andrea Kallumadyil. Andrea is from Ontario, Canada and is a medical student from UMHS. She is currently the president of Because We Care and the vice president of the American Medical Student Association at UMHS.
In this post, Andrea bravely shares her journey with PCOS and the life lessons it has taught her along the way.
One of my earliest memories as a child is standing in the hallway with my Grade 3 teacher as I chugged three boxes of apple juice. My Mom picked me up soon after, and I was to have my first ultrasound in a nearby city later that day. The week before, I had my first period. Being of South Asian descent, my family was beyond excited that I had “become a woman” at 8. We spent the afternoon, to my embarrassment, calling up relatives in India announcing the good news. My parents took me out to a nearby convenience store, where I picked out a gift to celebrate the big day. On our way home, we stopped at the walk-in clinic to make sure everything was okay. Practising in a small town with predominantly white patients, my doctor had never had a patient have their period so young. She assumed it could be explained by my South Asian background but decided to run some tests just in case it was something else. The healthcare staff poked and prodded me, only for the tests and ultrasound to come back normal. I was sent home and did not have another period for four years.
I got my period again when I was 12 years old. My periods seemed to have a mind of their own. They would come and go as they please – but they were consistently heavy, caused me a lot of pain, and lasted at least a week. A few months into this unpredictable cycle, I had a period that was more than 30 days long. I was pale, and my hands and feet were freezing in the middle of the summer. They ran some blood tests and referred me to a gynaecologist. I was not only anaemic but also had high levels of free testosterone in my system. Given my lab values and symptoms, the gynaecologist had said it was a straightforward diagnosis: PCOS.
What is PCOS? What are the Symptoms?

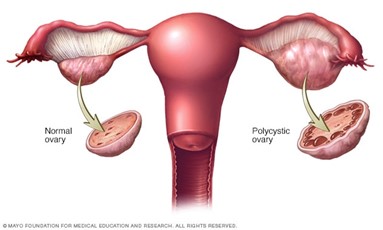
Polycystic Ovarian/Ovary Syndrome is an endocrine (hormonal) disorder that affects the normal functioning of your ovaries. The three main features are
- Ovary Dysfunction: Presents as irregular periods, including infrequent periods, prolonged periods, and an absence of periods.
- High levels of androgen: Determined either with a blood test or via symptoms of hirsutism (excess body/facial hair) or acne. Androgens, although referred to as male sex hormones, are naturally occurring hormones at low levels in females.
- Cystic Ovaries: The collection of fluid in follicles preventing the release of an egg during your menstrual cycle (ovulation).
A patient usually requires at least two of the three main features to be diagnosed with PCOS. The different combinations give rise to 4 distinct PCOS phenotypes:
- Phenotype A: High levels of androgen, ovary dysfunction, and cysts.
- Phenotype B: High levels of androgen and ovary dysfunction
- Phenotype C: High levels of androgen and cysts.
- Phenotype D: Ovary dysfunction and cysts.
In my case, I had irregular periods and high levels of androgen shown both in my blood tests and excessive body and facial hair (hirsutism): Phenotype B. During your diagnostic process, your health care provider may also order an ultrasound and gynaecological exam to rule out other potential causes for your symptoms.
Hirsutism is hard to assess, especially since many populations – Middle Eastern, South Asian and Mediterranean – have more body/facial hair than other ethnic groups, despite having normal androgen levels. Being of South Asian background myself, and the only South Asian family in a then-predominantly white community, my hirsutism was initially overlooked. For many young persons with PCOS, including myself, this continues to be one of the most challenging symptoms to manage.
Outside of the 3 diagnostic features, PCOS has many other symptoms and complications, including:
- Infertility: PCOS is one of the most common causes of infertility due to less frequent ovulation. It can also increase the risk of pregnancy complications like gestational diabetes and miscarriage.
- Weight Gain and Trouble with Weight Loss: Almost 80% of persons diagnosed with PCOS are overweight. Additionally, being overweight can make other PCOS symptoms even worse.
- Metabolic Syndrome: Those overweight and those with PCOS are at risk for insulin resistance leading to diabetes, high blood pressure, and high cholesterol levels. This puts those with PCOS at risk for developing heart disease – as many as 50% of persons with PCOS will have insulin resistance.
- Androgenic Alopecia: Excess androgen can cause hair loss on the head. Resembles male pattern balding.
- Acanthosis Nigricans: Dark and thick skin around the neck, breasts, armpits, and groin area
- Sleep Apnea: The risk is about 5-10 times higher for those with PCOS. This is primarily because those with PCOS are likely to be overweight.
- Depression, Anxiety & Disorders: Hormonal changes along can increase the likelihood of experiencing depression. Symptoms like hirsutism can increase this risk.
- Endometrial Cancer: The lining of the uterus (endometrium) is at risk of developing cancer if you are insulin resistant, overweight or have trouble ovulating – all of which are PCOS features.
Treatment

With each additional symptom, my doctor explained, I felt myself becoming more and more ostracized, imagining all the new ways I’d look even more different from my friends in my hometown. The racing images came to a halt when I heard the word infertility. I was too shocked to process the rest of the information I received and was frankly too embarrassed to ask any questions about what I did hear. I was prescribed an oral contraceptive for my irregular cycles and Vaniqa (a topical hair growth inhibitor) for my hirsutism and left the office. When we got in the car, my Mom asked if I was okay, and in response, I cried the entire 45 minutes home.
I wish I knew that although PCOS is one of the most common causes of infertility, it is also one of the most treatable. There are many options available to manage the symptoms of PCOS.
- Oral Contraceptive Pills: OCPs help regulate hormone levels and foster regular, predictable periods that are shorter in duration with a lighter flow.
- Metformin: A diabetes drug that improves insulin resistance, can promote weight loss, reduces the rate of miscarriage, and promotes regular menstrual cycles.
- Spironolactone: An androgen medication that can be used to lower androgen levels in your body. This will improve symptoms of androgenic alopecia, hirsutism, and hormonal acne.
- Hair Removal: Once hormone levels are managed, many people have success with electrolysis – the only truly permanent hair removal solution. A probe is inserted into each hair follicle to destroy each hair’s growth centre. Other less permanent methods include laser hair removal, epilation, threading, sugaring/waxing, or depilatory creams. A hair growth inhibitor like Vaniqa can also be used, but the hair will resume growth if you cease usage.
- Weight Loss: Losing up to 5-10% of your body fat can be enough to kick start ovulation. There is also some evidence that a low carb diet may improve your hormone levels and increase fertility. A healthy lifestyle consisting of nutritious foods and exercise will enhance fertility treatment effectiveness regardless of weight loss – remember, it is highly recommended to consult a health care provider before making any significant lifestyle changes.
- Acupuncture: There is some emerging evidence that acupuncture procedures restore LH and FSH hormone ratios and promote regular menstrual cycles in those with PCOS.
- Surgery: A laparoscopic procedure that involves destroying a part of the ovary with an electric current. This can stimulate ovulation and decrease androgen levels. The results last for a few months.
-
For those trying to get pregnant, additional treatment options include:
- Fertility Drugs: Clomid is a fertility drug that triggers ovulation and is often used in combination with metformin. Although some persons can become resistant to the drug, Letrozole (a cancer drug) has shown to be effective in stimulating ovulation in such situations. Injectable gonadotropins are also available under different brand names to stimulate ovulation. However, those with PCOS are at a high risk of developing ovarian hyperstimulation syndrome. Furthermore, you are also at increased risk for multiple pregnancies.
- Intrauterine Insemination (IUI): A process involving sperm placement in the uterus with a catheter. This process is known to increase the total number of sperm that reach the fallopian tubes.
- In Vitro Fertilization (IVF): After stimulation of egg production, multiple eggs are removed and inseminated in a lab dish. Multiple embryos are transferred a few days later back into the uterus.
There is also evidence that the following supplements can relieve some symptoms of PCOS. They include:
- Myo-inositol: Reduces the risk of gestational diabetes
- Inositol: Increases the number of ovulations, thereby leading to a higher chance of successful conception.
- Omega-3 Fish Oils: Lowers total cholesterol levels.
- Co-Supplementation of Magnesium, Zinc, Calcium, and Vitamin D: Provides beneficial effects on hormone levels while reducing inflammation and oxidative stress caused by PCOS.
Living With PCOS

Being diagnosed and starting treatment at a very young age, I was fortunate to not have to deal with the unpredictability of irregular periods. However, I did struggle with managing my hirsutism. I started laser hair removal almost immediately after my diagnosis and embarked on a process that would last several years. I bleached most of my body hair to feel comfortable wearing revealing clothes. I eventually switched to electrolysis, which did reduce the amount of hair grown by 30% but was incredibly painful and time-consuming. I considered myself a very anxious person but was officially diagnosed with anxiety and depression at the beginning of my undergraduate degree. I quickly gained a lot of weight following a high-stress period and my hirsutism got much worse as a result. I went on the keto diet to lose it and obsessively worked out.
However, a restrictive lifestyle like that was not sustainable for me and did not promote good mental health. I was still terrified that I would never have kids and am to this day very set on a specific timeline in my head. I initially set aside my career goals of becoming a physician for something attainable in a shorter period. I bounced from counselling to nursing to speech-language pathology. I did every possible prerequisite during my bachelor’s degree to keep all of my options open. I read countless blogs and videos of what other persons with PCOS did for family planning, careers, and managing their symptoms. I realized that everyone had their own unique story and that the only commonality is that they all did what made them happy. Those that wanted to start a family were able to do so without compromising their career goals. From then on, I began to focus on what I wanted instead of letting my PCOS control every little detail of my life. I stopped being so hard on myself for having symptoms. I started to wear short sleeves without bleaching, I got into the program I wanted to get into, and most importantly, I began to accept myself for who I am. It has been such a freeing experience.
For those currently struggling with PCOS right now:
- Try not to compare yourself to anyone else.
- Work on what is best for you, given your own story.
- Learn to be comfortable in your skin.
- Talk to your health care provider to figure out the best way to manage your symptoms.
- And most importantly: do not let anyone convince you that your PCOS can stop you from doing whatever you set your mind to.
****
We would like to say a big thank you to Andrea for being so open and bravely sharing her PCOS story. If you’d like to ask her a question, please leave it in the comments section below or you can email your question to info@lakehealthandwellbeing.com
Sources
- D’Anna, R., Di Benedetto, V., Rizzo, P., Raffone, E., Interdonato, M. L., Corrado, F., & Di Benedetto, A. (2012). Myo-inositol may prevent gestational diabetes in PCOS women. Gynecological endocrinology : the official journal of the International Society of Gynecological Endocrinology, 28(6), 440–442. https://doi.org/10.3109/09513590.2011.633665
- Alois, M., & Estores, I. M. (2019). Hormonal Regulation In Pcos Using Acupuncture And Herbal Supplements: A Case Report And Review Of The Literature. Integrative Medicine (Encinitas, Calif.), 18(5), 36-39.
- Arentz, S., Smith, C. A., Abbott, J., & Bensoussan, A. (2017). Nutritional supplements and herbal medicines for women with polycystic ovary syndrome; a systematic review and meta-analysis. BMC complementary and alternative medicine, 17(1), 500. https://doi.org/10.1186/s12906-017-2011-x
- Lizneva, D., Suturina, L., Walker, W., Brakta, S., Gavrilova-Jordan, L., & Azziz, R. (2016). Criteria, prevalence, and phenotypes of polycystic ovary syndrome. Fertility and sterility, 106(1), 6–15. https://doi.org/10.1016/j.fertnstert.2016.05.003
- Maktabi, M., Jamilian, M., & Asemi, Z. (2018). Magnesium-Zinc-Calcium-Vitamin D co-supplementation improves hormonal profiles, biomarkers of inflammation and oxidative stress in women with polycystic ovary syndrome: a randomized, double-blind, placebo-controlled trial. Biological trace element research, 182(1), 21–28. https://doi.org/10.1007/s12011-017-1085-0
- Polycystic Ovary Syndrome (PCOS). (2020). Retrieved 16 October 2020 from https://www.mayoclinic.org/diseases-conditions/pcos/symptoms-causes/syc-20353439
- Polycystic Ovary Syndrome. (2012). Retrieved 16 October 2020 from https://americanpregnancy.org/womens-health/polycystic-ovary-syndrome-70990
- Polycystic Ovary Syndrome. (2019). Retrieved 16 October 2020 from https://www.womenshealth.gov/a-z-topics/polycystic-ovary-syndrome
- Polycystic Ovary Syndrome. (2019). Retrieved 16 October 2020 from https://www.healthlinkbc.ca/health-topics/tw9103