Dispelling myths about SSB Taxes
While SSB taxes are found to be effective at reducing purchases and consumption of SSBs and producing better public health outcomes in the long run, different counter-arguments are made in resistance to this tax-based health policy. One common argument made by industry stakeholders against SSB taxes is that they will lead to considerable job losses among businesses that produce, distribute and sell the taxed beverages; however, these claims are unfounded.
To date, peer-reviewed SSB tax evaluation studies have estimated labour market impacts in taxing jurisdictions of the United States and these studies consistently found no net negative impacts on employment and unemployment outcomes. No evidence of net job losses or job losses in industries that produce or sell SSBs has been found (UIC, 2022). Rather, SSB taxation may influence market development by sparking the growth of a healthy drink and food industry. By increasing awareness of the harms of high-sugar diets and utilizing SSB tax revenues to subsidise local fruits and vegetables, the local fruit juice market stands to benefit from expansion and sustainability. Small businesses and street vendors who sell SSBs can make and sell local unsweetened fruit juices and healthy snacks where the demand for healthier and cheaper drink alternatives increases as a result of SSB taxation.
Conclusion
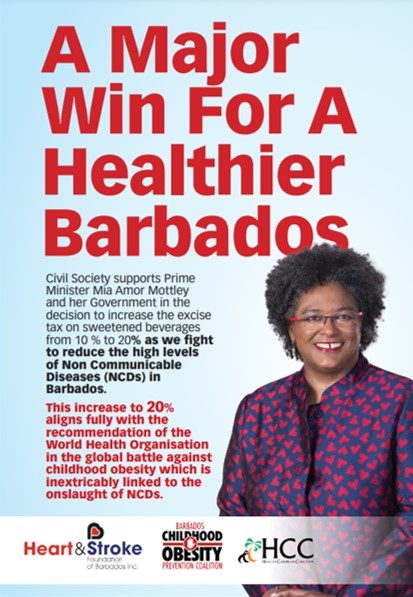
Now more than ever, civil society organisations (CSOs) across the world are advocating for effective health policies, like SSB taxation, that help to improve health outcomes and cultivate healthy environments for all. SSB taxes are demonstrably effective at reducing SSB purchases and improving obesity rates in the long term. To achieve the greatest impact in NCD prevention and control, taxation ought to be coupled with other policies that help to reduce socioeconomic inequalities in diet-related health.
Interventions such as including front-of-pack warning labels, cultivating healthy school environments through nutrition education, implementing sale restrictions on sugary foods and drinks in schools and at hospitals, and providing subsidies on locally grown healthy foods are all valuable and necessary for the most equitable impact on consumer behaviour and health outcomes. To combat the threat that NCDs pose on our people, productivity and livelihoods, government, civil society, industry, individuals and communities must work together. Together we can strengthen calls to action for local government to prioritise proper health, nutrition and wellbeing by implementing health policies that lead to better health and sustainability for all.