Category: Non-Communicable Diseases (NCDs)
The Unexpected Burden of Multiple Myeloma


Aaron discusses the emotions and challenges faced by caregivers of patients with multiple myeloma. By recounting his mother’s experience as a caregiver, he identifies barriers that a caregiver may struggle with and provides scientifically supported practical advice to help those who have recently become caregivers of a loved one with multiple myeloma.
Cancer is a group of diseases that everyone is familiar with in some form. Formally, it is the uncontrolled replication of cells leading to various problems. One particular cancer that will be the focus of this post is multiple myeloma (MM). Specifically, we will focus on the caregiver burden of those caring for someone with MM, as there is a lack of emphasis on their well-being and personal experience, but first, a bit of background information.
What is MM? MM is a type of blood cancer that is progressively debilitating, painful and ultimately fatal (most commonly due to infection).
Who is at risk? It occurs 1.6x more often in males than in females. It is 2x as often in the Black population than in the Caucasian population. Additionally, Black people are more likely to get it at a younger age.
When is it usually diagnosed? The median age of diagnosis is 65 years old. In cases diagnosed and treated early, 60% of patients will survive up to 5 years; only a fraction will survive 10 years after diagnosis.
What causes it? While there is a confirmed genetic role, there is also evidence of many other factors contributing to its onset. Such factors include exposure to radioactive substances and certain chemicals, such as benzene. Usually, a large dose of benzene can only be acquired from being exposed to factory emissions for several years or wastewater.
What are some symptoms? MM has systemic complications ranging from severe bone pain/ osteoporosis to kidney failure and infection. Throughout the progression of the disease and administration of treatment, it is standard to see periods of remission, periods of high severity and periods where the side effects feel worse than the disease.
Can it be treated? Sadly, the majority of people with MM will pass away. Recovery is possible if the patient is diagnosed early and started on therapy. Treatment ranges from conventional chemotherapy to stem cell transplantation. You can find more information on how these treatments work on the American Cancer Society’s website.
Unfortunately, MM patients are often misdiagnosed or are diagnosed late because there is a lack of experience diagnosing it among physicians. The latter happened with my grandfather, and within 1 year of diagnosis, he passed away. While many understand the suffering of a cancer patient, not many understand the challenges the caregivers face; a role that my mother fulfilled for my grandfather. A caregiver is someone responsible for the needs of the patient, often without any compensation. Responsibilities of a caregiver include scheduling, transport, finances, housekeeping, legal support and emotional support. It is usually a spouse, adult, child, or other immediate family members that fill this role and the role of a caregiver can be simultaneously rewarding and challenging.
My mother had her own mix of such emotions as a caregiver. At the time of my grandfather’s diagnosis, we had already lived in Canada for 10 years and in the United Arab Emirates before that, while my grandparents were living in India. Although my mom would go to India over the summers to look after my grandparents, she was otherwise dependent on friends and relatives to ensure my grandparents’ health and safety. The inability to be there with them for longer left her with a sense of guilt at the end of each summer, especially the last summer before my grandfather’s death. The uneven sharing of the caregiver role among family had placed an enormous strain on some of these relationships
As a caregiver, it is essential to note that uncertainty is the greatest obstacle for the well-being of both the patient and the caregiver. A caregiver’s well-being often reflects the status of the patient. Studies have identified numerous challenges to caregiver well-being. Most caregivers face at least a few of these challenges:
- Initial shock: After having to endure the path to diagnosis, eagerly awaiting results, the confirmation of a diagnosis for any type of cancer will come as a shock. Additionally, caregivers must adapt by changing their lifestyles and take on new responsibilities to support their loved ones. Part of the difficulty is due to the unpredictable course of the illness. Many patients and caregivers must endure the shock several times as the disease re-surfaces. Lack of knowledge about the disease is an enormous source of stress.
- Commitment: Being a caregiver sometimes involves giving up your previous lifestyle to reserve free time for an emergency and patient care logistics. Logistics include, but are not limited to, finances and housekeeping (which change as the course of the disease changes).
- The emotional sphere: Caregivers often have feelings of anxiety and fear. Patients often feel that they are burdening their caregivers and relatives with their condition. Caregivers have been found to have a similar attitude, not wanting to burden others with the responsibilities or emotional baggage that comes with being a caregiver. Consequently, they suffer by themselves, unable to honestly express their feelings while being afraid to leave the patient to have well-deserved self-care. They often experience spiritual suffering, unable to find finding meaning in the disease.
As a medical student who is always looking for ways to help people, I have found many coping strategies backed by evidence that worked for my mother and other caregivers. The following is a list of strategies, that as a caregiver, may help you provide the best possible care while looking after your own well-being:
- Ensure that you have a list of questions you can ask the doctor when going in for a visit. Make sure you cover the diagnosis, progression and what to expect, types of treatments, treatments in clinical trials, and end-of-life and palliative care. A full list of questions can be found at the National Cancer Institute. If possible, ask the hospital to send the results home before meeting up with the doctor to help you take in the news and develop better questions.
- Establish your support system. Rather than bottling up emotions and avoiding burdening others, try to connect with others, spread the responsibility, and the emotional burden with close relatives or friends.
- Know your support services. Joining a support group is an excellent resource for information on handling caregiver responsibilities, treatment options, possible side effects, warning signs, etc. It is also a safe space where you can vent your thoughts to those able to relate and learn from others about their coping strategies.
- Keep doing the things you enjoy. It’s okay to leave the patient in the care of someone else for a few hours or a day so you can recuperate. It will only help you become a better caregiver and help you remember your loved one with fondness rather than as a burden.
- Use mindfulness meditation and improve emotion-regulation. These will help you prepare for the hard days and the death of your loved one.
Understanding and anticipating the challenges will allow you to avoid some of the anxieties associated with caregiving and better manage your time so you can spend it with your loved one. Keep in mind that every caregiver-patient relationship is different. There is more than one way to be a great caregiver. I hope the strategies above (which are by no means an exhaustive list) will go a long way in promoting caregiver well-being physically, emotionally, and spiritually.
More Support
We’re aiming to support multiple myeloma patients and their family members through the JAA Fund. Small support grants are currently available for patients in St Kitts, Nevis, the British Virgin Islands, Trinidad and Tobago. If you’ve been affected by multiple myeloma, live in one of these countries and require some financial support, you can apply for a grant here
References
Aksoy, M., Erdem, Ş., Dinçol, G., Kutlar, A., Bakioğlu, I., & Hepyüksel, T. (1984). Clinical Observations Showing the Role of Some Factors in the Etiology of Multiple Myeloma. Acta Haematologica, 71(2), 116-120. doi: 10.1159/000206568
Howell, D., Hart, R., Smith, A., Macleod, U., Patmore, R., Cook, G., & Roman, E. (2018). Myeloma: Patient accounts of their pathways to diagnosis. PLOS ONE, 13(4), e0194788. doi: 10.1371/journal.pone.0194788
Monterosso, L., Taylor, K., Platt, V., Lobb, E., Musiello, T., & Bulsara, C. et al. (2017). Living With Multiple Myeloma. Journal Of Patient Experience, 5(1), 6-15. doi: 10.1177/2374373517715011
Multiple Myeloma. (2020). Retrieved 11 September 2020, from https://www.cancer.org/cancer/multiple-myeloma.html
Quiñoa-Salanova, C., Porta-Sales, J., Monforte-Royo, C., & Edo-Gual, M. (2019). The experiences and needs of primary family caregivers of patients with multiple myeloma: A qualitative analysis. Palliative Medicine, 33(5), 500-509. doi: 10.1177/0269216319830017
Waxman, A., Mink, P., Devesa, S., Anderson, W., Weiss, B., & Kristinsson, S. et al. (2010). Racial disparities in incidence and outcome in multiple myeloma: a population-based study. Blood, 116(25), 5501-5506. doi: 10.1182/blood-2010-07-298760
The Joan Ajose-Adeogun Fund Aims to Support Multiple Myeloma Patients
The Joan Ajose-Adeogun fund is being established in loving memory of Joan Ajose-Adeogun who sadly passed away from multiple myeloma on 11th September 2019. Her diagnosis of multiple myeloma was devastating and within months Joan had lost her ability to speak and walk, her brain function and was in unbearable pain.
Understanding the many challenges that patients and their families face, we are raising funds to support multiple myeloma patients.
Grants will be available to help improve the wellbeing of patients and their families and will cover some of the costs of:
- Home care
- Medical facility/care home fees
- Retreats and respite breaks for patients and their families
- Palliative care
- Psychological support and counselling for patients and families
- Brain stimulation therapy
- Treatment and medication
- Physiotherapy
- Transportation costs (for family members to visit patients and specialised transportation for patients)
- Equipment such as wheelchairs, stairlifts, healthcare beds
- Bathroom adaptions and other required home adaptions for patients
- Patient’s utility bills
- Doctor’s appointments
- Medical treatment abroad
Priority will be given to patients residing in St Kitts, Nevis, the British Virgin Islands, Trinidad and Tobago, Nigeria and Ghana, countries that were near and dear to Joan’s heart.
How you can help?
We would be delighted if you would make a donation to support this cause and ensure that those affected by multiple myeloma can receive the support that they need during a very traumatic, devastating and difficult time.
You can also invite your friends to make a donation or have some fun and host a fundraiser – a cake sale, fundraising party, dinner or gala, an auction, a sponsored run or walk, a coffee morning; the sky is the limit.
We’d love to hear from you so please do leave a comment in the section below to share your experience with multiple myeloma, your reason for donating and to share any fun fundraising events you’ve organised.
Thank you
Thank you for your support, let’s make a difference together.
If you’d like to be kept up-to-date with our progress, please sign up to our newsletter here.
Fund Management
This fund will be managed by Lake Health and Wellbeing, a registered NGO in St Kitts and Nevis, and financially reviewed annually by Pelican Accounting and Business Services.
Online payments are being managed by JAD Cash, a comprehensive e-money solution for the Eastern Caribbean countries. All online payments will, therefore, be processed in Eastern Caribbean Dollars (XCD). Please note that $1 USD = $2.7 XCD and £1 = $3.40 XCD.
Up Next
In our next blog in this series, we’ll be discussing what multiple myeloma is.
Mesothelioma Isn’t Going Anywhere
Today, we’re delighted to share a guest blog post from the team at Mesothelioma Guide. Mesothelioma Guide connects mesothelioma patients and their loved ones to top doctors, cancer centres and treatment options, plus legal resources. In today’s feature, they dispel the myth that the asbestos-related cancer, mesothelioma, has been eradicated since the introduction of legislation restricting the use of asbestos.
In the latter half of the 20th century, the general public learned of asbestos’ dangers. They learned the substance is, in fact, a carcinogen, one which can lead to aggressive diseases such as mesothelioma.
The awareness of asbestos’ harm led to increased regulations worldwide and scrutiny of businesses which used the mineral. Most people expected asbestos-related diseases like mesothelioma to level off early in the 21st century and eventually fade into obscurity.
This has not happened — nor will it any time soon.
According to the World Journal of Surgery, pleural mesothelioma cases in the United States increased from 2004 to 2014. The World Health Organization revealed that around 43,000 people worldwide die from this cancer. Despite more than 60 countries banning the commercial use of asbestos, the mesothelioma mortality rate has increased worldwide since the 1990s. This is proof that mesothelioma isn’t going anywhere.
National Cancer Database on Mesothelioma
In 2004, there were 1,783 pleural mesothelioma cases in the United States. In 2014, there were 1,961 reported cases. That’s an increase of around 10%.
Pleural mesothelioma accounts for between 70% and 80% of all U.S. mesothelioma cases and the same is true globally. Peritoneal mesothelioma and pericardial mesothelioma comprise the other 20-30% of cases.
According to numerous sources, including the Centers for Disease Control and Prevention, there are usually between 3,000 and 3,300 new mesothelioma cases in the U.S. each year. From 2012-2016, there were on average 3,253 new cases each year. In 2016 alone, 3,096 mesothelioma cases were reported.
The World Health Organization estimates that 10,000 new mesothelioma cases each year are diagnosed collectively in Australia, Japan, North America and western Europe.
In the United Kingdom, the incidence of mesothelioma has increased steadily each year from the 1950s (153 cases) to 2010 (2,360 cases). Like we said earlier, this disease isn’t going away.
But…
Mesothelioma Treatment Is Improving
Science continually evolves, which means treatment for diseases continuously improves. Mesothelioma treatment is getting better, which is good news for patients and their loved ones.
Earlier in 2019, The U.S. Food and Drug Administration approved the Novo TTF-100L medical device for pleural mesothelioma treatment. It is limited to humanitarian use device distinction, but this approval was a significant moment for mesothelioma patients and doctors.
Peritoneal mesothelioma treatment is expanding as well. Many patients receive cytoreductive surgery, plus heated intraperitoneal chemotherapy (HIPEC) immediately after the operation. In a study published by the Annals of Surgical Oncology, around 55% of participants who underwent this treatment combination survived for at least three years. Roughly 37% survived for at least five years.
This study only included a few peritoneal mesothelioma patients, and other studies have reported different percentages:
- Between 50% and 65% for three-year survival
- Between 35% and 47% for five-year survival
Mesothelioma Patients Undergoing Treatment More Often
The best route to healing from mesothelioma is undergoing treatment. Surgery is the first choice followed by chemotherapy and radiation. If more patients receive medical help, then more of them will survive longer.
In 2004, treatment and survival rates in the U.S. were as follows:
- Approximately 34% of pleural mesothelioma patients underwent treatment.
- Around 37% of them survived for at least one year after diagnosis.
- Roughly 9% survived for at least three years.
In 2014, the rates were better:
- Around 54% of mesothelioma patients received treatment.
- Roughly 47% survived for at least one year after diagnosis.
- Approximately 15% survived for at least three years.
So, more people are getting treatment for their mesothelioma, and more people are surviving for longer after diagnosis.
How to Find Mesothelioma Treatment
We at Mesothelioma Guide can help patients find quality treatment and potentially extend their lives. Our patient advocate and registered nurse, Jenna Campagna, has connections to the top cancer centres in the USA.
If you or a loved one has mesothelioma, remember that treatment now is better than ever before. Jenna works with patients every day to improve their quality of life and prognosis. Email her at jenna@mesotheliomaguide.com if you wish to explore your treatment options.
More Information
If you have any questions on mesothelioma or would like any further information, you can leave your question for Mesothelioma Guide in the comments section below. Alternatively, you can visit Mesothelioma Guide’s website here, like their Facebook Page or follow them on Twitter.
Sources
- Largely Unchanged Annual Incidence and Overall Survival of Pleural Mesothelioma in the USA. World Journal of Surgery. Retrieved from: https://link.springer.com/article/10.1007s00268-019-05132-6. Accessed: 08/23/2019.
- Global mesothelioma deaths reported to the World Health Organization between 1994 and World Health Organization. Retrieved from: https://www.who.int/bulletin/volumes/89/10/11-086678/en/. Accessed: 04/22/2020.
- Global mesothelioma epidemic: Trend and features. Indian Journal of Occupational and Environmental Medicine. Retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4280782/. Accessed: 04/22/2020.
- Update on the management of malignant peritoneal mesothelioma. Translational Lung Cancer Research. Retrieved from: http://tlcr.amegroups.com/article/view/23788/18535. Accessed: 08/23/2019.
- Effect of Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy on Quality of Life in Patients with Peritoneal Mesothelioma. Annals of Surgical Oncology. Retrieved from: https://www.ncbi.nlm.nih.gov/pubmed/31069554. Accessed: 05/16/2019.
- Survival prognostic factors in patients undergoing cytoreductive surgery and hyperthermic intraperitoneal chemotherapy treatment: analysis from a single oncological center. WorldJournal of Surgical Oncology. Retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4815060/. Accessed: 04/12/2019.
Our Healthy Kids SKN Campaign
Non-communicable diseases (NCDS) like cancer, diabetes and heart disease are a major challenge in St Kitts and Nevis. Data has demonstrated that NCDs are becoming an epidemic in the Federation with 83% of deaths being due to NCDs. We must do something about this to prevent our citizens from dying prematurely.
One approach to tackling NCDs is to focus on the next generation and ensure that children adopt a healthy lifestyle. We have to create a healthy environment at schools, in homes and within society so that children can make healthy choices.
Our Healthy Kids SKN campaign aims to raise awareness of the changes that children need to make in order to reduce their risk of developing an NCD later in life. We’re encouraging children, parents and teachers to focus on three main areas – eating healthily, drinking healthily and physical activity.
Eating Healthily
Junk food is everywhere so we must make a concerted effort to help children resist temptation and eat healthily. Children should eat a variety of foods to ensure they are getting enough nutrients to develop and grow. This includes consuming foods from all food types. In particular, parents should ensure that their children cut down on foods that are high in sugar, salt and saturated fat and introduce more fruits and vegetables into their diet.
Children should eat 5-7 portions of fruits and vegetables every day, and eat colourfully, and aim to eat different colours of fruit and vegetables.
Drinking Healthily
Children in the Caribbean drink large quantities of sugary drinks putting them at risk of becoming obese or overweight. Caribbean children’s frequency of consuming sugary drinks was found to be amongst the highest out of 187 countries. Furthermore, teenagers (12 to 15-year olds) in Barbados, Jamaica, the Bahamas and Trinidad and Tobago reported drinking sugary drinks three times or more a day, and in St Kitts and Nevis, it was found that children consumed at least one carbonated soft drink a day.
Soft drinks are very high in sugar, for example, a can of coke contains 9.75 teaspoons (39g) of sugar and even juices contain high levels of sugar, a 330ml box of Rica Orange Juice contains 10.6 teaspoons of (42.2g) sugar – that’s more than coke!
We’re encouraging children to cut out the sugary drinks and drink water instead.
Physical Activity
For children to get healthy, they need to be active every day. The World Health Organisation recommends that children accumulate 60 minutes of moderate to vigorous-intensity physical activity every day.
We must get creative about physical activity as in St Kitts and Nevis, children are not active enough, over half of children, 58.4%, are physically inactive. We need fun approaches that don’t feel like work.
Working With Young People
We’re delighted to have worked with a young designer, Hadiya Lewis, to create the three graphics for this campaign. This is a great example of the talent and creativity that exists and how young people can contribute to communicating important health messages.
SKN Moves Support
We’re delighted that this initiative has been endorsed by SKN Moves and we’d like to thank the SKN Moves team for their support.
You can find out more about SKN Moves here
Final Chronic Disease Self-Management Course of the Year
Signed, sealed, delivered and it’s a wrap! On Tuesday 26th November 2019, we completed the final session of our six-week chronic disease self-management course. This was our third and final workshop of the year. In April 2019, we held our first 6-week course, and this was followed by our second one in August 2019.
This final set of workshops began on 22nd October with a class of 13, all-female and whose ages ranged from 25 to 60.
We had a dynamic group of ladies who were keen to learn, very willing to participate and share their health stories and experiences and support each other; this created a great atmosphere for learning and built a strong sense of camaraderie.
Over the six weeks, we covered a number of self-management techniques such as action-planning, physical activity, problem-solving, decision making, healthy eating, medication management, communication skills and more.
Through group work, brainstorming sessions and homework, the course material came to life for participants and they were able to apply what was learnt each week to their own personal situation.
During our weekly feedback sessions, it was very rewarding to hear the impact the self-management techniques had made in just a short space of time and to hear of how each topic caused participants to reflect on their lifestyle and make a commitment to make healthier choices.
As usual, the section on food labels caused quite a stir when participants realized the quantities of sugar, salt and fat in many of the items they consume and this was a bit of a wake-up call with participants making small changes like switching to skimmed milk and reducing their portion sizes.
Once again, we found facilitating this course to have been a very rewarding experience and look forward to hosting more of these courses next year.
We’d like to say a big thank you to everyone who attended the course. We know it was a significant time commitment and we appreciate your dedication, time and your willingness to get involved.
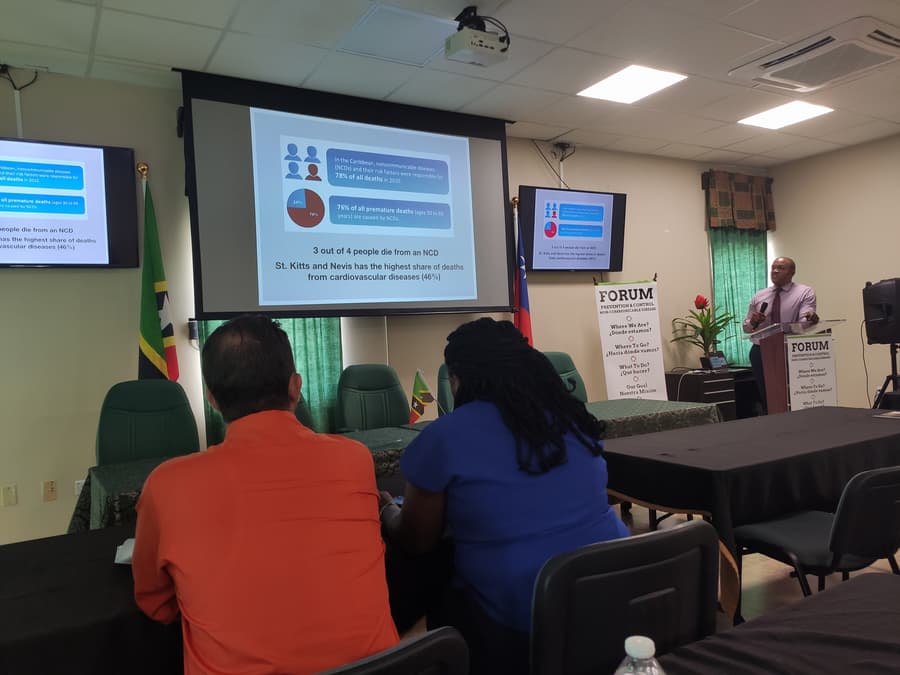
St Kitts and Nevis Forum for Chronic Disease Prevention and Control
On 14th November 2019, we were delighted to have been able to attend the Forum for Chronic Disease Prevention and Control which was hosted by the Taiwan International Cooperation and Development Fund in partnership with the Ministry of Health in St Kitts and Nevis.
This event aimed to bring together both local and international organisations working in the field to share their experiences, present their work and thus provide a platform to learn, share best practices, promote regional collaboration and identify the best way forward in tackling chronic diseases in St Kitts and Nevis.
This was a very important event as chronic diseases are a major cause of death in St Kitts and Nevis – 83% of deaths in the Federation are due to chronic diseases. Therefore, the prevention and control of these conditions is a major priority for the Ministry of Health and the ICDF is working towards supporting the government to strengthen its non-communicable disease (NCD) strategy.
Over the three days of the forum, in attendance were representatives from CARPHA, the Ministries of Health of Belize, St Vincent and the Grenadines and St Kitts and Nevis; the JNF Hospital in St Kitts; the St Kitts Diabetes Association, Community Health Centres in St Kitts and Nevis and the Taipei Veterans General Hospital.
We attended on the second day of this event. The theme for the day was: ‘Chronic Disease Management – Where to Go?’ This was an excellent and informative day featuring presentations from:
- Dr Bichara Sahely, Consultant Physician, Internal Medicine, JNF Hospital, St Kitts
- Dr Aljay Pierre, Medical Officer, Internal Medicine, JNF Hospital, St Kitts
- Dr Wei-Cheng Tseng, Taipei Veterans General Hospital
- Dr Hazel Laws, Chief Medical Officer, Ministry of Health, St Kitts
- Dr Marissa Carty, NCD Program Coordinator, Ministry of Health, St Kitts
- Mr Feng-Ta Tsai, Project Manager, Taiwan, ICDF
Together, the speakers provided an overview of the position around NCDs and made recommendations for what is required going forward if we are to effectively reduce the burden caused by NCDs. The take-home message of the day was the need for a greater focus on NCD prevention as most countries in the Caribbean will not be able to address NCDs with medical care alone.
The event ended with a very lively Q&A and panel discussion, giving the audience the opportunity to engage with the speakers and collectively explore solutions to addressing NCDs.
We very much enjoyed attending this event and found the presentations from Dr Sahely and Dr Pierre, particularly insightful. They both provided a very interesting perspective from doctors working on the frontline at the JNF Hospital to diagnose, treat and support patients. They highlighted that there is much work to be done in the Federation and this will involve improvements and changes to the system to facilitate prevention, early diagnosis, better management of patients with NCDs and an improvement in the quality of care delivered.
We look forward to playing our own very small part in tackling NCDs and would like to thank the ICDF and Ministry of Health for organising this event.
We Facilitate Our First Six-Week Chronic Disease Self-Management Course
From 2nd April to 7th May 2019, we facilitated our first chronic disease self-management course in St Kitts giving us the opportunity to support members in our community who have been affected by non-communicable diseases (NCDs).
Data has demonstrated that NCDs are becoming an epidemic in St Kitts and Nevis with 83% of deaths in the Federation being due to these conditions. To prevent these premature deaths and ensure that those living with an NCD can live well and have a good quality of life, support, information and guidance are required.
Providing patients with self-management skills is an effective and empowering way to ensure that those affected by a chronic disease can take control and improve their health and wellbeing. The Chronic Disease Self-Management Course helps us achieve this outcome.
The course that we facilitated is part of the Stanford University Chronic Disease Self-Management Program (CDSMP). This is an evidence-based prevention and health promotion program that addresses common issues faced by people with chronic conditions. The program has been implemented in 19 countries showing several benefits including:
- Improved wellbeing
- Improved health of participants
- Fewer hospitalisations
- Fewer days spent in hospital
Last year, we took part in the CDSMP training program which was delivered by the Ministry of Health in St Kitts. We were honoured to have come through the process and are now certified CDSMP facilitators allowing us to implement a free program of support for members in our community with an NCD.
Over the six-week period from the 2nd April to 7th May, we were delighted to guide our 18 participants through key self-management techniques. These techniques included action planning, problem-solving, decision making, medication management, communication skills, pain management, healthy eating, physical activity and more.
What we like about the course is that it is very interactive. Participants had the opportunity to take part in various activities, share their experiences, learn from one another and support each other. There was also homework every week to ensure that participants could start practising their self-management techniques immediately in their day-to-day life. It was wonderful to see and celebrate their successes every week.
We had a very engaged group who were a pleasure to work with. They got involved, asked questions and were keen to make the necessary changes in their lives to improve their health.
Facilitating this course has been one of the most rewarding experiences we have had in a long time. It was so touching to hear participants share how their lives have been impacted by the course. We look forward to seeing them continue to make great progress in taking control and more effectively managing their health.
A big thank you to everyone who attended and if you live in St Kitts and have been affected by a chronic illness like diabetes or high blood pressure and would like to attend a chronic disease self-management course, please do get in touch with us by email or call 765 8702
Our next 6-week course is due to start in July, all are welcome to attend.
“Thank you for the life lessons you have shared. Anyone who attends this course will never be the same again. The teachings will always be on one’s mind and heart. We must make a change! Eating, exercising and managing our lives better and being in control, this is an awesome feeling” – CDSMP Course Attendee
Discussions on Managing Conflict of Interest in NCD Prevention and Control in the Caribbean: Part 2
Welcome to part two of our ‘Discussions on Managing Conflict of Interest’ blog. In part one we provided some background to conflict of interest (CoI) and the challenges faced by those aiming to tackle NCDs in the Caribbean. Here, in part two, we’ll be providing highlights from the Health Caribbean Coalition’s (HCC) conflict of interest meeting which we attended a couple of weeks ago.
The HCC’s Meeting
The HCC’s CoI meeting was a two-day regional event held on 26th and 27th March 2019 that had a focus on conflict of interest in the prevention and control of non-communicable diseases (NCDs) in the Caribbean, and the overall aim of the meeting was to begin to build regional capacity to identify and manage conflict of interest.
Regional Experiences of Conflict of Interest
The meeting started with an interesting and insightful look at regional experiences of CoI from both civil society and the public sector. From civil society, we heard from the Heart Foundation of Jamaica, the HCC and the Trinidad and Tobago Heart Foundation, and from the public sector, we heard from representatives from the Ministries of Health in Antigua, the Bahamas and Jamaica. Collectively they touched on industry interference and conflict of interest. Some interesting points that were raised included:
- In the Caribbean, in most instances, we have to live with CoI and so approaching this area from the point of view of managing CoI is a more practical and realistic approach
- The difficulty of dealing with the “smallness” of the Caribbean – everyone knows each other and in our professional lives, in tackling NCDs, we may have to fight against people we know and respect
- Absolutes are unlikely to work except with the tobacco industry where globally the public health community does not partner with tobacco companies. For other industries, like the food and beverage industry, we must explore degrees of conflict of interest (low, medium and high) and degrees of partnership or engagement. Not every engagement will be detrimental to public health and we must understand how to manage conflict of interest whilst getting the most benefit out of any relationship or partnership
- What happens after a conflict of interest has been identified? What is the process for review? Is it an actual, potential or perceived CoI? What is the process for recusal?
- Should an organisation’s CoI policy be generic or specific?
- Some good practice with respect to disclosure forms:
- All CoI policies should have a supporting disclosure form
- Disclosure forms are valid for a year
- The obligation is on the person who is disclosing to report any changes within that year
- Have a process for checking the accuracy of a completed disclosure form
- Managing conflicts of interest – ensure that if you’re going into a partnership with industry that a lawyer reviews the MoU and any non-disclosure agreements to prevent any CoI issues; don’t be afraid to negotiate so you can minimise any risks or exposures.
WHO/PAHO Tool for Preventing and Managing CoI In Nutrition


The PAHO scoping tool provides a simple method to evaluate potential engagements and is divided into three areas that enable organisations to reflect on important issues before deciding on whether to enter into an engagement with an external entity. These areas include:
- Actor alignment
- Engagement profile
- Assessing the risk and benefits
Additionally, this scoping tool complements the more comprehensive decision-making tree developed as part of the WHO draft tool. This is a 6-step process that takes the user through a structured process for analysing a potential engagement to identify and manage conflict of interest. The steps include:
- Exploring the rationale for engagement
- Profiling, due diligence and risk assessment of the external actor and the potential engagement
- Balancing risks and benefits
- Risk management
- Monitoring, evaluation and accountability
- Transparency and communication
Both resources provide users with an objective and comprehensive method of identifying and assessing conflict of interest, whether an engagement should be pursued and if so, what measures can be introduced to manage any conflicts of interest.
The HCC’s CoI Guide and Policy
Finally, the HCC presented their draft CoI guide and policy which is aimed at their staff, volunteers, board members, advisors, interns and consultants. Their policy and guide aims to prevent, identify, avoid and manage CoI. It also aims to serve as a general guide for civil society organisations and individuals as they develop their own CoI policies, the idea being that CSOs can simply adapt the HCC policy to suit local needs and situations.
Our Thoughts
We thought this was an excellent meeting which gave us a lot of food for thought.
Conflict of interest is an area that we considered on a simple level, but this meeting allowed us to explore this subject in depth and fully appreciate the risks of not properly analysing the relationships that we seek to enter.
The meeting was very timely as over the past few months we’ve started to explore organisations that we can approach to support some of our activities and during this process, we have found it challenging to determine whether we should pursue forming relationships with an organisation that promotes both healthy and unhealthy food and beverages. Attending this meeting has given us some clarity and by using the knowledge we have gained from this meeting and the PAHO tool we believe we can make a better decision.
Conclusion
We encourage Caribbean civil society organisations working in the NCD field to explore developing an approach to tackling conflict of interest to safeguard the credibility and integrity of their work, and for further information, please do reach out to the Healthy Caribbean Coalition
Discussions on Managing Conflict of Interest in NCD Prevention and Control in the Caribbean: Part 1
On 26th and 27th March 2019, we joined representatives from across the Caribbean in attending the Healthy Caribbean Coalition’s workshop on conflict of interest (CoI). This event had a special focus on conflict of interest in non-communicable disease (NCD) prevention and control in the Caribbean.
This is going to be a two-part blog and in today’s piece we’re going to provide some background to conflict of interest and in part two we’ll provide some highlights from the HCC’s CoI meeting.
What is Conflict of Interest?
The World Health Organisation describes conflict of interest as:
“…circumstances where there is potential for a secondary interest to unduly influence, or where it may be reasonably perceived to unduly influence, either the independence or objectivity of professional judgement or actions regarding a primary interest.”
They also explain that:
“The existence of conflict of interest in all its forms does not as such mean that improper action has occurred, but rather the risk of such improper action occurring. Conflicts of interest are not only financial but can take other forms as well.”
Another definition of CoI comes from Public Health and Food and Beverage Industry Engagement: A Tool to Guide Partnership Opportunities and Challenges. They define CoI as:
“… where one engages in any private, personal or business undertaking or other activity in which one’s private or personal interest conflicts with one’s duties or responsibilities…”
For further clarity around the concept of CoI further explanations have been offered which categorise CoI into perceived, potential and actual and these are defined as follows:
- An actual conflict of interest occurs when there is a direct conflict between a person’s professional duties within an organisation and a competing interest or obligation, whether personal or involving a third-party.
- A potential conflict of interest arises where a person has an interest or obligation, whether personal or involving a third-party, that could conflict with their professional duties and responsibilities in the future.
- A perceived conflict of interest occurs where it could reasonably be perceived, or give the appearance, that a competing interest could improperly influence a person’s professional duties.
Additionally, CoI may be seen at the individual, institutional and structural levels.
By understanding and reflecting on these definitions we can recognise if we, or our organisation, may be conflicted. This will allow us to take steps to address this to ensure we are serving our primary interest – this is the one we committed to serve at the outset of our professional journey (in our case, improving the public’s health).
Conflict of Interest, the Caribbean and NCDs
Small Island Developing States (SIDS) like the Caribbean are presented with a unique set of circumstances which make the area of conflict of interest particularly challenging. The circumstances in question relate to the very small populations creating an unavoidable, overlapping, intertwined social and business environment. This means that individuals and organisations may have multiple competing interests. Therefore, staff working in organisations aiming to prevent and control NCDs may, at some point, find themselves in a number of difficult situations when it comes to CoI. This may include:
- Having a family member, friend or close associate working in an industry that produces products that are risk factors for NCDs
- Being offered funding, sponsorship or resources from companies that produce unhealthy products in a landscape where there are very limited funding and sponsorship opportunities
- Exploring a partnership with a company that produces both healthy and unhealthy products
- Being invited to take part in health campaigns by companies who produce products that are risk factors for NCDs (with there being no other companies to partner with to reach such a large audience)
- Developing NCD prevention and control policies with individuals and entities who have competing interests
In larger countries there are multiple options when there is a need to partner with individuals and organisations to implement projects to prevent and control NCDs so many of the above situations can be avoided. Therefore, their approach to conflict of interest centres on prevention.
In Small Island Developing States, many of these conflicting situations cannot be avoided so not-for-profit entities (as well as government departments) have to start to re-think their approach to conflict of interest, focusing on strategies to effectively manage conflict of interest.
The HCC’s Conflict of Interest Meeting
Historically, conflict of interest, in many cases, has been addressed with a global blanket approach that doesn’t delve into the complex, overlapping business and personal relationships as well as the challenging funding environment that exists in the Caribbean. A more bespoke approach is needed for the Caribbean and hence the HCC’s conflict of interest meeting brought organisations together for in-depth discussions on this issue. Time was also set aside to explore solutions through the review and testing of a new conflict of interest tool being developed by WHO/PAHO as well as the review of a conflict of interest policy and guide being developed by the HCC. This meeting was very informative and we were delighted to have attended.
Coming Up Next Time
In part two of this blog we’ll summarise the highlights from the meeting, but in the meantime, for further information on conflict of interest you can explore the documents in our reference list below. We also encourage anyone working in public health in a Small Island Developing State to develop an approach to managing CoI to ensure the credibility and integrity of their organisation remains intact.
References
- The Healthy People and Communities Steering Committee’s Multi-Sectoral Partnerships Task Group, 2014. Public Health and Food and Beverage Industry Engagement A Tool to Guide Partnership Opportunities and Challenges, Ontario, Canada: The Healthy People and Communities Steering Committee’s Multi-Sectoral Partnerships Task Group, May 2014.
- University of Southern Queensland. Conflicts of Interest. [Online]. Available at <https://www.usq.edu.au/hr/empcond/conflicts> [Accessed on 3rd April 2019]
- WHO, 2016. Framework of Engagement With Non-State Actors. [Meeting Proceedings] 28th May 2016. Sixty-Ninth World Health Assembly.
- WHO, 2015. Addressing and managing conflicts of interest in the planning and delivery of nutrition programmes at country level. Report of a technical consultation convened in Geneva, Switzerland, on 8–9 October 2015.