We Talk Stress Management and Healthy Lifestyles During Verchilds High School’s Health and Wellness Week
From 29th April to 3rd May 2019, the counselling department at Verschilds High School hosted their Health and Wellness Week and we were delighted to have been invited to take part in two of their planned events.
On 29th April, we spoke, bright and early, at the school’s assembly on the topic of stress management. During our 15 minute presentation, we talked about what stress is, what types of situations cause stress, the impact of stress and how we can manage stress.
We encouraged students to think about their own personal situations, especially during this exam period, to see how they can address any stressors that may be affecting their wellbeing and provided tips on managing these, which included – identifying stressors, elimination/delay of stressors, preparation, stress relief techniques, building resilience and getting support.
We had a great session with the student body and therefore were very happy to return on the 3rd May for their health and wellness fair.
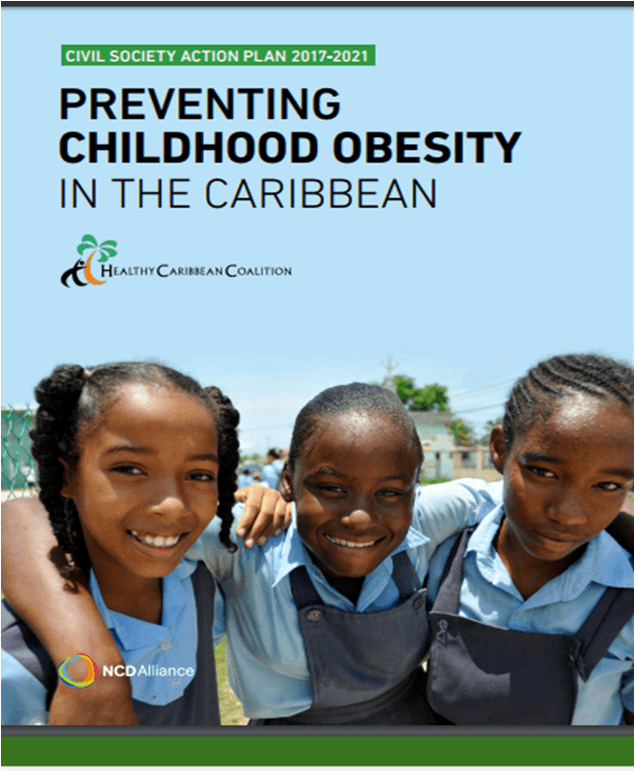
During their health and wellness fair, we set up a stall and promoted living a healthy lifestyle. We spoke to students and staff about the importance of children and teenagers getting enough exercise and physical activity (WHO recommends 60 minutes per day), drinking more water, eating 5-7 portions of fruit and vegetables per day and cutting down on sugary drinks.
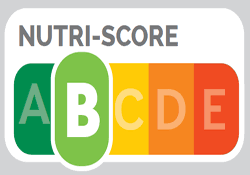
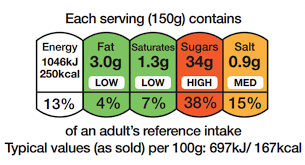
We had information showing how much sugar is in many popular soft drinks and students and teachers were shocked to learn that one can of coke contains 8 teaspoons of sugar.
To encourage children to swap their unhealthy snacks for healthier snacks, we had some lovely mangoes for staff and students to sample and this included some dried mangoes. Dried mango is a great alternative to candy and chocolate and it tastes great – the students (well…most of them) loved it.
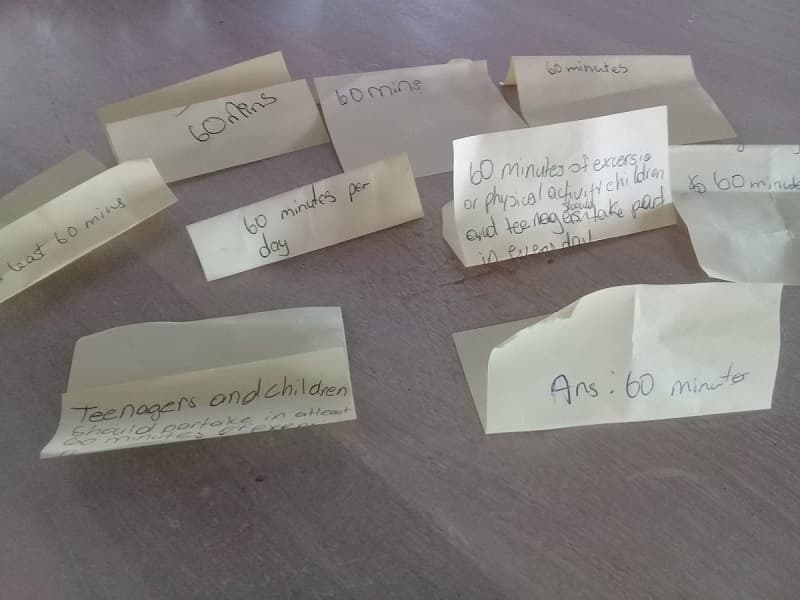
We also held a competition where we asked students how many minutes of physical activity children and teenagers should take part in every day and three lucky students won a comic book – congratulations.
Finally, it was great to connect with the other stallholders, some of whom were familiar faces, such as the team behind Mother Becky Bush Tea and Sugar Town Organics. It was nice meeting the Gideon Force Organic Agriculture Cooperative, Close to Nature and the Drugs and Substance Misuse Team and learning about the great work they are all doing.
We had a great time at Verchilds High School and would like to thank the staff for their kind invitation and both staff and students for their warm welcome, visiting our stall and asking some great questions.