At the end of last year we conducted a prostate cancer engagement pilot project as part of a large piece of work funded by Prostate Cancer UK to determine the most effective method of reaching the black community with the key messages about prostate cancer.
Local charities were invited to apply for funding to carry out small projects over 3-4 months and we applied for funding to focus on black churches to determine whether, in reality, this is an effective and practical environment to raise awareness of prostate cancer.
Targeting black churches has two main advantages. Firstly, if we take London as an example, a large number of London’s black population attends church regularly. The London Church Census, covering the time period 2005-2012, found that 48% of inner London’s church goers and 21% of outer London’s church goers were black1. Based on their figures this equates to 238,158 people from the African and African Caribbean community. This means that by targeting black churches we can reach a significant proportion of the African Caribbean community.
The second advantage of targeting churches is that it provides a very structured environment where a large number of people meet regularly. This, in theory, makes it a convenient environment to deliver health awareness messages. Additionally, many churches have developed their institutions beyond just preaching on a Sunday. Many churches have Men’s Fellowships, Young Professional Networks, Women’s Fellowships, Over 50’s Clubs, Men’s Conferences, Women’s Conferences and social functions. This means that there is the opportunity, in some churches, to select a sub-population within a church that would most benefit from a particular health message.
Whilst there are advantages to targeting black churches there are some logistical challenges. Firstly, churches tend to have a busy programme of events that will have been planned months in advance making it difficult to fit additional events into their schedule. Secondly, the ideal situation would be to deliver a presentation on a Sunday where there is access to the entire congregation, but many churches may not be able to accommodate this. This means that awareness presentations would have to be delivered on a Saturday or during the week where only a small percentage of the congregation is likely to attend. Through a flexible approach, being creative with the methods of engagement and developing long term relationships with churches it is possible to overcome some of these challenges.
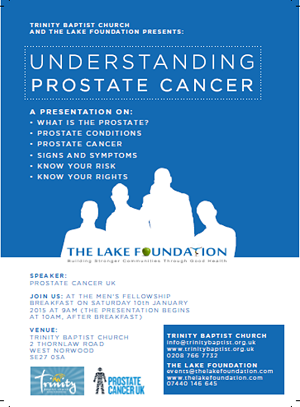
The Lake Foundation being based in Croydon, where there is a diverse population and a significant number of black churches, decided to work locally and target churches in Croydon and the surrounding area. In our pilot we worked with two churches and explored the best strategy for working with churches to raise awareness amongst their congregations.
From our pilot we found that:
- Engaging with black churches can be an effective way of reaching the African Caribbean community with the key messages about prostate cancer because of the potential of reaching large numbers.
- To reach large numbers in a church setting requires the development of a long-term bespoke engagement programme.
- There is a need to understand the structure of individual churches to ensure the best strategy is implemented to reach as many of their members as possible.
- Engaging with churches may include targeting Sunday services for maximum reach and/or organising awareness sessions on a weekday/Saturday to ensure members have a more in-depth knowledge of prostate cancer.
Recommendations
Overall The Lake Foundation recommended that Prostate Cancer UK explores developing a structured awareness program for African Caribbean churches in the UK or contracting this work out to community organisations. Whilst this may require significant time, personnel and resources we believe it is an effective way of reaching the black community.
Our specific recommendations:
Target Sunday Services
This pilot has shown that targeting Sunday services would ensure large numbers of people are reached but with limited information because of the time constraints of fitting into the Sunday service’s programme
Targeting churches successfully on a Sunday would require two approaches:
- A short presentation during all their Sunday services
- Setting up an information table throughout the day on a Sunday
Specific recommendations:
- Develop a 5-7 minute presentation that could be used for Sunday services
- Develop an easy method to measure the impact of delivering short presentations at a Sunday service
- Be flexible and persistent
Target churches outside of a Sunday service to achieve depth of knowledge
If the aim is to deliver in-depth information about prostate cancer to church goers and if this isn’t possible through a Sunday service due to time constraints then an additional approach will need to be taken.
The pilot has shown that targeting churches through a one-off event (not on a Sunday) is not the most effective method of reaching the largest number of people, this only reaches a small percentage of a church’s congregation. Therefore a regular engagement programme is needed.
Specific recommendations:
- Work with individual churches to understand their structure and how best to reach their members
- Identify groups, departments, events and forums within individual churches that can provide an effective environment to raise awareness
- Organise regular events with the same church throughout the year
- Make good use of churches’ communication platforms – social media, website, newsletters, bulletins, TV stations, YouTube channels etc.
We believe that by taking a long-term, flexible and creative approach in targeting churches a significant impact can be made and we’re delighted to learn that Prostate Cancer UK will be launching a new Faith Based Outreach Project using what we learnt from this pilot. We wish them all the very best in this project and hope that is makes a significant difference in increasing cancer outcomes by facilitating early diagnosis and we’d like to thank Prostate Cancer UK for giving us the opportunity to conduct this pilot.
You can download our full report below.
References
1. Brierley Consultancy, London Church Census and London City Mission, 2013. London’s Churches are Growing.Kent: Brierley Consultancy