Our Fibroids Publications
Through our fibroids publications, we aim to provide useful, simple and straightforward information on fibroids. We have produced a fibroids booklet, reviewed by healthcare professionals and women with fibroids; are creating a series of fact sheets on areas that women have highlighted are important to them and have also produced a report summarising a small piece of research we conducted to explore the needs of black women with fibroids.
Booklets and Reports
Understanding the Needs of Women with Fibroids
We conducted some research to understand the experience of African and African-Caribbean women with fibroids. This work explored the needs of women with fibroids and determined if women had access to enough information and support. Our findings then informed the development of our fibroids information and support programme.
You can read our report here.
Publication date: 21st January 2015
Redesign: July 2019
Our booklet provides much-needed information on all aspects of fibroids from symptoms and risk factors to treatment and prevention. It aims to ensure that women have accurate, reliable information about fibroids. We hope this booklet will be a one-stop-shop for anyone with questions or concerns about fibroids.
You can read the booklet here.
Publication date: 29th July 2015
Our booklet will be updated in 2020
Fact Sheets
Fibroids and Exercise – in this fact sheet we discuss how exercise may help with alleviating symptoms and provide readers with simple tips on how to get active without aggravating their current symptoms.
Updated: March 2019
Download here: Fibroids and Exercise Fact Sheet
Acknowledgements: We’d like to thank Candice Bryan from Noire Wellness for contributing to this fact sheet and Way Wive Wordz Publishing, Editing and Tuition.
Fibroids and Your Emotional Wellbeing: this fact sheet aims to help women identify, understand and address the emotions that may be associated with having fibroids.
Updated: April 2019
Download here: Fibroids and Your Emotional Wellbeing
Acknowledgements: We’d like to thank Olivia Haltman from OH Counselling Services for co-authoring this fact sheet and Way Wive Wordz Publishing, Editing and Tuition for editing this document.
Infographics
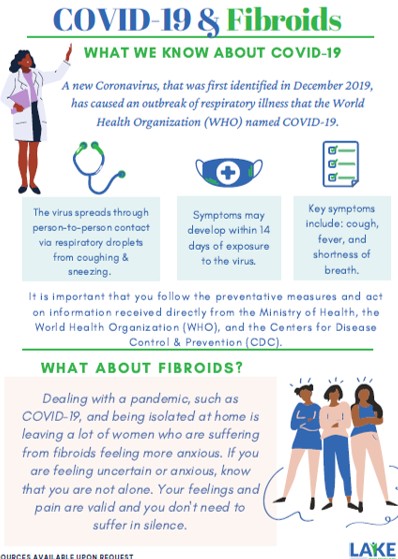
Fibroids and COVID-19: this comprehensive infographic explores how the COVID-19 pandemic may be affecting fibroids patients and provides some self-care and stress management tips to help women cope during this challenging time.
Published: 18th May 2020
Download here: Fibroids and COVID-19 Infographic
Reviewed by: Dr Oduntan, District Medical Officer, St Kitts and Nevis
You can download a list of the references used to prepare this infographic here
We would like to thank our volunteer, Mariana Ndrio, a second-year medical student at the UMHS in St Kitts and Nevis for her hard work in preparing this resource.
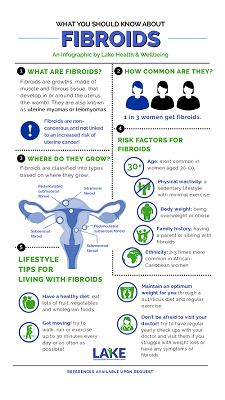 What You Need to Know About Fibroids: This infographic provides an overview of fibroids covering what fibroids are, the different types, risk factors, prevention tips and symptoms.
What You Need to Know About Fibroids: This infographic provides an overview of fibroids covering what fibroids are, the different types, risk factors, prevention tips and symptoms.
Published: 1st June 2020
Download here: What You Need to Know About Fibroids
You can download a list of references used to prepare this infographic here
We would like to thank Dr Sofia Miah, who recently graduated from the University of Exeter Medical School, for her hard work in preparing this infographic.
This infographic was reviewed by a UK-based gynaecologist.
We are committed to making all our resources free and easily accessible to all those who need it. You can help us with this commitment by making a donation which will go towards the costs of producing our health information which includes the costs of design, printing and editing. You can make a donation here. Thank you for any help that you can provide.
Please note that our online payments are being managed by JAD Cash, a comprehensive e-money solution for the Eastern Caribbean countries. All online payments will, therefore, be processed in Eastern Caribbean Dollars (XCD)